(RNS) — Trust in secular U.S. health care institutions has been in free fall. In 2022, Gallup found that only 38% had a “great deal” or “quite a lot” of confidence in our medical system. Back in 1968, that number was 73%. The crisis is particularly acute among young people, those with less education and people of color. The mistrust deepens significantly when it comes to government health agencies, whether federal, state or local.
Medical communities have had a particularly bad track record when it comes to disability. Physicians consistently rate the quality of life of their disabled patients lower than those patients do themselves. This gap sometimes results in certain disabled patients being denied end-of-life care given to healthier patients.
People of color, especially disabled Black Americans, have expressed a particular distrust of the care they are given. The infamous 2020 case of Michael Hickson, a Black man who had been paralyzed after a brain injury, gave us a window into why. A recording taken by Hickson’s wife revealed a white doctor insisting that they forgo intubation for COVID-19 because Michael’s quality of life argued against it.
When Hickson’s wife pointed to other brain-injured patients who were getting treatment, the doctors explained that they “were walking and talking people.” It’s little wonder that Black Americans have a deep distrust of end-of-life medical practices that extends to skepticism about physician-assisted suicide and even hospice.
Now, an exploding debate over brain death promises a new chapter in this struggle.
Until the 1960s, the idea that an individual could be fighting off infections, responding to bodily trauma with an increased heart rate and release of adrenaline and even successfully gestating a child to birth and yet be considered dead was still quite strange. But in 1969, the Harvard Brain Death Commission, motivated by the fact that so many people were dying while waiting on organ transplant lists, invented the concept of “brain death.” The idea was that if one’s brain had died, the body was closer to a corpse (animated by machines and drugs) than a living, self-integrating human being. That body could therefore be freed up to donate vital organs for transplant.
Debates have followed about whether the brain is, in fact, necessary for an individual to be a considered a living person. (Some evidence suggests that, especially in children, the spinal cord can take over for functions of the brain.) But almost everyone thought, per the Harvard committee’s conception, that the brain-death standard meant that the whole brain — not just part of it — had to be dead.
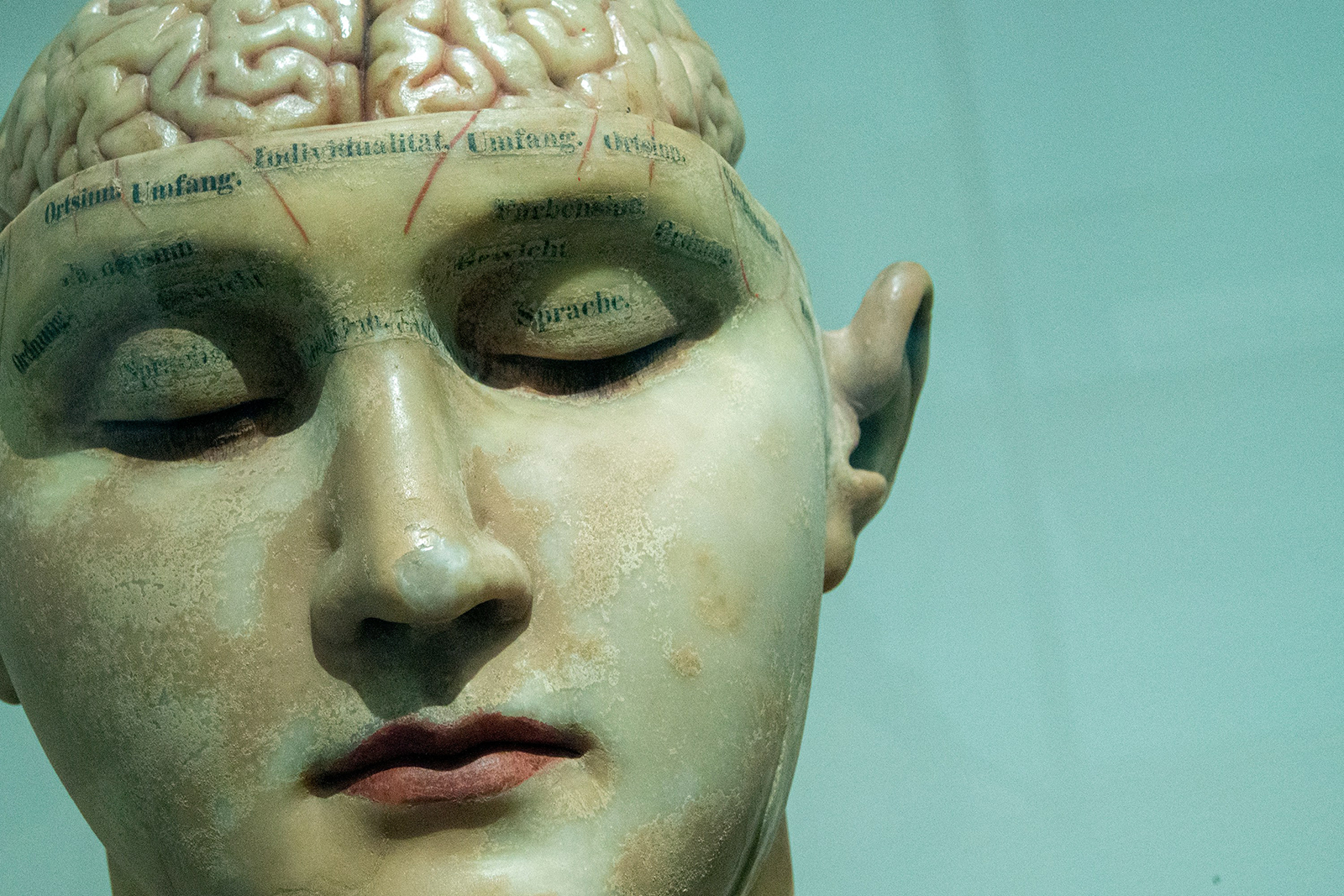
(Photo by David Matos/Unsplash/Creative Commons)
This is the language the Uniform Law Commission, a quasi-governmental agency that works to bring conformity to U.S. state laws, proposed in the early 1980s and that is now the law in the overwhelming majority of states: Brain death and the death of the human being were indicated by “irreversible cessation of all functions of the entire brain, including the brain stem.”
Over time, however, this consensus has eroded. An unsigned 2009 editorial in the medical journal Nature, for instance, admitted that most physicians weren’t testing for whole brain death and insisted that someone with only part of their brain stem still functioning “will never again be the person he or she was.”
In part because providers and institutions were ignoring the brain-death statutes, the commission met last summer to explore whether it should propose a new definition of death. As an observing member of that committee, I can attest there was no consensus on anything. Views ranged from wanting to ditch the concept of brain death altogether to insistence that what matters is not the death of the brain at all, but rather loss of capacity for consciousness. The commission rightly ended its work by deciding that no uniform language could be proposed.
Enter the American Academy of Neurology, which, only weeks later, published a “Consensus Guideline” on brain death. But AAN’s report admitted that “Because of the lack of high-quality evidence on the subject, a novel, evidence-informed formal consensus process was used.” In sum, the AAN’s experts voted on a definition of brain death while intentionally excluding from the vote “those whose profession and intellectual bias would diminish the credibility of the guideline in the eyes of the intended users.”
The AAN’s supposed consensus rejected “whole brain death” language, replacing it with concern for functioning of the “brain as a whole.” Specifically, AAN claims the whole brain does not need to be dead; instead, some neuroendocrine function (such as in the hypothalamus) can persist and a human being still be declared dead.
This was the definition that led Jahi McMath to be declared dead by her home state of California — before she later reached puberty and had her first period! Another Black victim of U.S. end-of-life practices, she would go on to live for five years in an apartment in New Jersey, the only state in the union that takes religious freedom (and therefore the wishes of McMath’s parents) into account on these matters.
This vision of death is obviously incompatible with both common sense and with the explicit views of multiple religious traditions. The National Catholic Bioethics Center has already said that it is incompatible with the church’s teaching, and it was New Jersey’s Orthodox Jews who pushed to carve out the religious freedom exemption in their state that allowed McMath to be cared for and not discarded as California intended.
All of this has received very little coverage in the media. As a result, some states’ adoption of AAN’s standard has gone largely unnoticed. Nevada, for instance, decided to adopt the AAN’s standard without review. The New York state Department of Health recently posted on its website, without public comment or review, that it is accepting the AAN standard, flatly contradicting New York state law, which insists on “irreversible cessation of all functions of the entire brain, including the brain stem.”
Any state that naively adopts the AAN standard, especially via a nonlegislative process, should face legal challenges, not only because it may violate local statutes. Human beings with catastrophic brain injuries have precisely the same dignity as able-bodied human beings, and describing them as “dead” so they may be used for their organs is deeply offensive. Doing so may also be illegal under both the Americans with Disabilities Act of 1990 and the religious freedom provisions of the Civil Rights Act of 1964.
If states use the AAN’s brain-death standard, it will mean that some patients will be declared both brain-dead and “actually” dead when they are neither. Motivated by the wish for organ donation, secular medicine is engaged in a culture war against human dignity and equality, in which it is finding new ways to discard patients who are disproportionately economically vulnerable and from historically marginalized communities.
It is time to stand up and be heard and hold the medical communities to account in defense of the least among us.






